By Benjamin Ryan
NBC News
“Harlem United’s Preston Wholly said he works with his clients who have contracted the virus to cut through the harmful stigma tied to contracting monkeypox.
“‘We really want to process that it wasn’t their fault and work through the guilt and shame and kind of normalize it,’ he said.”
During the four months of the monkeypox outbreak, health care providers, researchers and an anxious public have scrambled to determine how the virus transmits, how to prevent it and how the infection plays out in the body.
Little attention has been paid to what comes after the infection clears.
Following recovery from this skin lesion–causing virus, people often find themselves waiting anxiously over the course of months to see whether monkeypox will leave them with permanent scarring. And in interviews with more than a dozen people who have had the virus and as many health care providers and researchers, NBC News learned that in some people, the lingering scars are not only physical but psychological. Troublingly, it’s also possible the virus could cause permanent damage to sensitive internal tissues and give rise to persistent pain or other onerous long-term symptoms.
“Just because you’re cleared and no longer contagious, it doesn’t mean you’re totally back to normal,” said Matt Ford, 30, a bicoastal actor who contracted the virus at the beginning of the summer and hopes that his scarring, including pockmarks on his face, will continue to dissipate. “It did a number on my body, especially in more sensitive areas.”
Unfortunately, people looking to doctors or health agencies for answers about what to expect post-pox are typically met with an information vacuum. This is the result of the notorious dearth of research conducted prior to the outbreak about a virus that until this spring largely only circulated in western and central Africa.
“I just want there to be more concrete information, but maybe that’s asking too much,” said Brad, 33, a New York City area resident who preferred to use only his first name to protect his medical privacy.
In an emailed statement, the New York City health commissioner, Dr. Ashwin Vasan, acknowledged this lack of health guidance, saying, “It’s still early in the outbreak and the kinds of long-term studies needed to understand these issues better have not been completed yet. We continue to learn from what people who’ve experienced infection and recovery are reporting.”
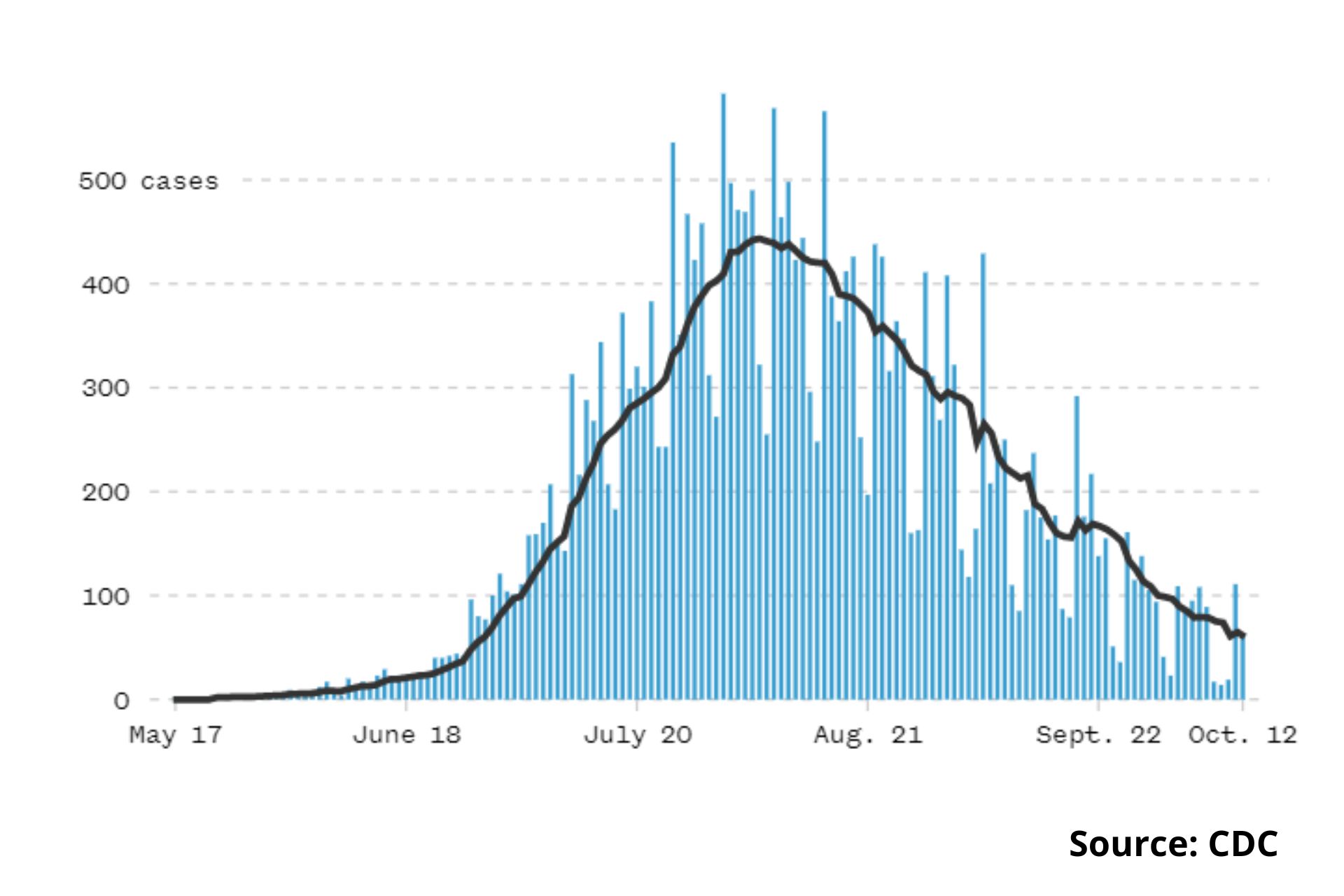
Since the unprecedented global outbreak was first detected by health authorities in mid-May, 65,415 cases have been diagnosed worldwide, 24,846 of them in the United States, the Centers for Disease Control and Prevention reports. While the weekly case count both nationally and worldwide has declined in recent weeks, raising hopes that the outbreak might be brought under control, concerns remain that at least a fraction of those who have had the virus might suffer long-term impacts of the infection.
Cosmetic concerns
For gay men, who comprise the overwhelming share of global monkeypox cases and among whom the competitiveness to look good is famously Olympian, worry over sustaining noticeable scarring in the wake of the infection can be particularly taxing.
“Especially for people who already have body dysmorphia or are hypersensitive to how others see them, there is this hypervigilance” of such cosmetic effects, said Preston Wholly, managing clinical director of behavioral health services at the LGBTQ-focused nonprofit health care provider Harlem United in New York City.
The marks are also signals of an infection that because it largely transmits through sex between men, can be highly stigmatized.
“I think it’s important to be aware of the effect of stigma regarding the route of monkeypox transmission, at-risk groups and disfiguring skin lesions — all of which could contribute to psychological distress,” said Dr. James Badenoch, a physician at the Queen Mary University of Medicine in London and the co-lead author of a paper published Sept. 8 in eClinicalMedicine on neurological and psychiatric conditions linked to monkeypox.
Harun Tulunay, 35, was hospitalized with a particularly severe case of the virus in July. In addition to experiencing extreme proctitis, or inflammation of the rectal tissues, and an inability to swallow, he developed an atypically large purple-black lesion that covered his entire left nostril. The lesion has since healed but has left behind pockmarked scar tissue.
“I am very obsessed with the little scar on my nose and am using lots of creams, scared it won’t go away,” said Tulunay, who, like a substantial proportion of people who contract monkeypox, has HIV.
Dr. Howa Yeung, an assistant professor of dermatology at the Emory University School of Medicine in Atlanta, said that while guidance on care for monkeypox lesions may be lacking, what is known about treating smallpox, which like monkeypox belongs to the orthopoxvirus family, can serve as a guide.
Yeung recommended the use of what are known as hydrocolloid dressings on lesions, which help keep them moist and promote healing while minimizing scarring. For thicker scars, silicone gel or patches may help improve their appearance, he said—especially if such treatment is started shortly after the scabs fall off. Later on, lasers and microneedling may further improve their appearance, although such interventions can be expensive.
The dermatologist noted that people with darker skin tones are likely at higher risk of monkeypox lesions leaving lasting dark marks, which he estimated could take three to 12 months to fade.
“Some scars will be permanent,” Yeung said.
He advised the use of skin-lightening agents, which a dermatologist can prescribe, as well as a high SPF sunscreen to keep the sun from further darkening the pigment.
Gerald Febles, 25, reported grappling with such marks, which, although they have been improving, still greatly bother him. Hoping they will recede over the coming months, he’s tried various scar-treatment creams, which don’t come cheap.
“I was very confident in my own skin before,” said Febles, who is an employee relations manager for the urgent care company MedRite. He said he now has “a lot more insecurity about my body in general. I’ve even gone to bars and some people have asked, ‘Oh, what’s that on your neck?’ So it’s something I’m reminded of whether or not it’s on my own terms.”
Febles was keen to assert that he sees no reason to be ashamed of having had monkeypox. But recalling that the infection caused him excruciating pain, he nevertheless characterized such questions from people as “a trauma trigger.”
The potential for lasting damage
Proctitis, experienced by 1 in 4 people with the virus in a Spanish study and 16% of U.S. cases about which the CDC has data, is one of the most devastating potential monkeypox symptoms. It can cause excruciating pain, in particular when defecating. What’s more, such symptoms might portend longer-term consequences of the infection.
During a July 14 Infectious Diseases Society of America call with reporters, Dr. Mary Foote, a medical epidemiologist at New York City’s health department, raised an early alarm that monkeypox lesions might cause permanent internal damage in some people. This, she said, could include the formation of scar tissue or strictures in the anorectal or urethral tissues, which could affect bodily functioning.
“It’s quite concerning,” Foote said of these potential outcomes, which she recently told NBC News might prompt the need for surgery or other interventions.
Dr. Boghuma Titanji, an infectious disease specialist at Emory University, reported seeing urethral damage or overall pain in the penis, including difficulty retracting the foreskin, due to scarring from monkeypox.
“When we see these cases with urologic involvement, we consult urologists,” Titanji said, noting that “early urinary catheterization and other interventions may prevent complications down the line.”
Brian Rice, 43, reported suffering from a host of bothersome health problems, including the flu, since recovering from monkeypox in mid-August. Having endured penile pain, swelling and discharge during the infection, the attorney has since experienced pain in his pelvic area and the frequent need to urinate. These symptoms eventually resolved themselves, Rice said, following pelvic floor myofascial release treatments. But he’s also experienced a persistent rash in his pubic area that is only recently starting to clear up.
“Nobody knows whether these other symptoms I’m experiencing are related in any way to monkeypox,” said Rice, who is HIV positive and lives in Cliffside Park, New Jersey. “It could be stress and anxiety; it could just be triggering other things.”
Dr. Peter Shalit, who runs an LGBTQ-focused primary-care medical practice in Seattle, reported that one of his patients had a mild case of monkeypox in July, with only skin lesions. Then, in August, the man relapsed and suffered from worse disease symptoms, including proctitis. Three weeks after recovering the second time, his rectal symptoms returned once more, causing him severe pain. Shalit treated both the second and third waves with the antiviral TPOXX, which appeared effective at battling symptoms.
The eClinicalMedicine paper published this month reported that in rare cases people with monkeypox develop neurologic symptoms, including encephalitis, confusion or seizures.
“Encephalitis can cause long-term problems with disability, mood and memory problems,” said Dr. Jonathan Rogers, a psychiatrist at University College London and a co-lead author of the paper. He stressed, however, that he and his coauthors don’t have the necessary follow-up data to determine any extended effects of this condition among people who have recovered from monkeypox.
The CDC reported Sept. 13 the cases of two previously healthy men in their 30s who after contracting monkeypox developed encephalomyelitis, or inflammation of the brain and spinal cord. The men have recovered from the infection, but a month after the start of their neurologic symptoms, they each still require an assistive device to walk.
A difficult transition
Arriving during the Covid crisis denouement, the monkeypox outbreak has triggered pandemic-related anxieties that had only recently begun to abate, by sending people with the virus right back into isolation for the few weeks the infection takes to resolve. And as they grapple with recovering from such a stigmatized virus, many of those who spoke with NBC News said it has taken time for them to regain their confidence and calm within the outside world — be that interacting with colleagues, seeing friends and family, or getting back into dating and sexual intimacy.
These people report having a particularly difficult time disentangling the misery of monkeypox from the joys of sex.
“I just feel like I lost my mojo,” said Harun Tulunay, who, similar to Febles, finds men constantly striking up conversations with him about monkeypox, especially given how much media coverage his case received.
“They don’t seem much interested in dating me after,” he said, ruefully.
In the meantime, Tulunay, who is a training and volunteer coordinator at the HIV nonprofit Positively UK, is trying to get his semen tested to determine if he might still harbor the virus. Monkeypox has indeed been found in seminal fluid, and the World Health Organization has recommended that men wear condoms for 12 weeks following recovery from monkeypox out of concern, pending further research, that the virus might remain in semen and be transmissible for that long.
John Farrey, 32, said what he missed most while isolating with monkeypox was going out dancing with friends. So he thought he’d be jazzed to jump right back onto the dance floor once he recovered.
But, the Brooklyn tech worker said, “I felt very terrified of my own skin” during the immediate aftermath of his infection. Being around other people, he said, “still felt unsafe.”
“It really took me a long time to be comfortable having close contact again,” Farrey said.
For Brad, the New Yorker, having monkeypox was “totally traumatic,” sending him off-kilter emotionally. He’s been struggling to regain his equilibrium since then. A scar on his penis has made him self conscious and has caused him to worry that sexual partners will ask intrusive questions about it.
“Then it’s ‘bye-bye mood,’” Brad quipped of such a scenario.
“I’m still kind of afraid of sex, because my last sexual experience resulted in this, and it still carries so much weight,” he said of contracting monkeypox. “Sometimes it turns into this source of shame that I’ve never experienced before about sex.”
Then there’s the question of when the body is once again ready for the rigors of intercourse. Proctitis, said Dr. Chris Beyrer, director of the Duke University Global Health Institute, “is going have a very big impact on subsequent sexual functioning” for those who engage in receptive anal sex.
“I think the question is: ‘When have you sufficiently healed?’” Breyer said—which, he acknowledged, “is not a question that people have good answers for.”
The importance of support
Given the traumatic ripple effects that monkeypox can unleash, experts highlight the need to provide people who contract the virus with support that doesn’t end when the scabs clear up.
“The anguish experienced by many patients cannot be underestimated. It can be a truly horrible time,” Dr. Hans Kluge, regional director of WHO Europe, said at an Aug. 30 news conference about monkeypox. He called for buttressing “both the physical and mental health of patients during the entire course of the disease, and after. It remains of critical importance.”
Harlem United’s Preston Wholly said he works with his clients who have contracted the virus to cut through the harmful stigma tied to contracting monkeypox.
“We really want to process that it wasn’t their fault and work through the guilt and shame and kind of normalize it,” he said.
Jeffrey Galaise, 41, who said he has persistent nightmares about the infection —“I imagine myself having pox and pain,” he said — is among the many people who have contracted the virus and then established their own support networks. He founded a Zoom-based monkeypox support group for people with the virus he met mainly through social media. This outlet, he said, has been invaluable as he tries to move on.
“I need to get back to my normal life,” said Galaise, who works for a New York City governmental agency. “It has certainly been a transition. I certainly think I’m getting there.”
Brad, who has also found a supportive community of others who have had monkeypox through social media, said he yearns to have the lingering physical and emotional effects of monkeypox behind him.
“I would like there to be a day when I don’t worry about this anymore,” he said. “I just want to be done with it.”
Originally published by NBC News on September 25, 2022.